TOA BAJA, Puerto Rico, Jan. 25, 2022 (GLOBE NEWSWIRE) -- CytoImmune Therapeutics, a clinical-stage immunotherapy company that is developing a novel class of natural killer (NK) cell-based cancer therapies, today announced a study published in Proceedings of the National Academy of Sciences (PNAS), demonstrating the importance and impact of PDGF-D signaling in enhancing IL-15-mediated human natural killer cell survival.
The study, which took place at City of Hope, a world-renowned cancer research and treatment organization, found that PDGF-D activates NK cells via its receptor, PDGFRβ, in an autocrine manner and contributes to IL-15-mediated NK cell survival. Results from the study suggest that inducing PDGF signaling in tumor-reactive NK cells should benefit NK cell expansion and persistence and contribute to the enhanced effector function in NK cell-based immunotherapies. Further, given the known role of PDGF-D secretion by tumors, these findings also suggest that this signaling pathway may contribute to the beneficial effects of engineered NK cells to further modulate the tumor microenvironment in certain cancers.
"Our study supports the role and the importance of IL-15 in NK cell therapy. We remain focused in our pursuit to expand the understanding of NK cells as a cell therapy treatment for patients with hard-to-treat cancers," said Michael Caligiuri, M.D., president of City of Hope National Medical Center and a study senior author.
City of Hope licensed several patent applications to CytoImmune to develop a portfolio of chimeric antigen receptor (CAR) NK cell therapies.
"We are excited to share this data on the role of PDGF-D-PDGFRβ signaling in NK cells' survival. This foundational data supports CytoImmune's engineering approach to enhance NK cells' survival by introducing secretory IL-15 into each NK cell. Our deep scientific understanding of the biology of the tumor-reactive NK cell gives us further confidence in our innovative NK cell therapy approach as a new treatment option for patients fighting cancer," said Christina Coughlin, M.D., Ph.D., Chief Executive Officer of CytoImmune Therapeutics.
"We are encouraged by these findings and look forward to continuing our work in order to enhance our technology further," she added.
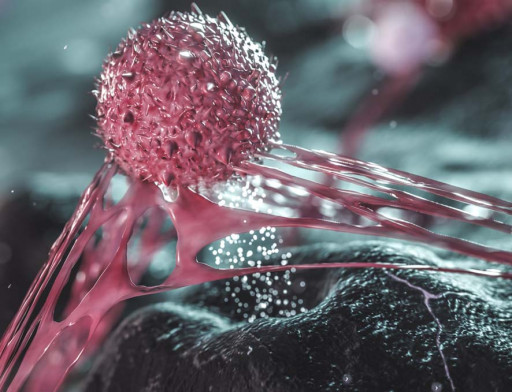
NK cell technology works by using NK cells from patients or normal donors. NK cells are then modified so they express certain genes (e.g., IL-15) to enhance survival and activation and a CAR that is specific for a protein expressed by cancerous cells. When the receptor binds, the NK cells become activated and destroy the cancerous tissue.
Based on Caligiuri and Jianhua Yu's research, who have over 55 years of collective laboratory investigation of NK cells, CytoImmune is developing an NK cell platform designed to overcome the limitations and challenges of current technologies. This collective knowledge and experience is utilized to engineer NK cells by focusing on the tumor-reactive NK cell subset.
The platform is designed to generate an abundant supply of CAR NK cells from a single donor with each cell engineered to express soluble IL-15 for sustained anti-tumor activity in the body. It will also enable scientists to freeze, transport and store engineered CAR NK cells for off-the-shelf use to treat cancer.
Please access here the study titled PDGF-D-PDGFRβ signaling enhances IL-15-mediated human natural killer cell survival. For more information please contact Will Rosellini: will@cytoimmune.com
About CytoImmune Therapeutics, Inc.
Founded in 2017, CytoImmune Therapeutics is a clinical-stage biotechnology company focused on developing an innovative and differentiated pipeline of NK cell therapies. It uses proprietary, robust, and well-characterized NK cell expansion and engineering technologies pioneered by Michael Caligiuri, M.D., and Jianhua Yu, Ph.D. The pipeline includes TRACK-NK for lung cancer, FLT3 CAR-NK for acute myeloid leukemia, PSCA CAR-NK cells for solid tumors and a GPRC5D BiKE-secreting BCMA CAR-NK cell for multiple myeloma. CytoImmune's lead product, CYTO-102 (TRACK-NK cell therapy), aims to enter the clinic in combination with atezolizumab (anti-PD-L1 monoclonal antibody) for non-small cell lung cancer in 2022.
Related Images
This content was issued through the press release distribution service at Newswire.com.
Attachment